EFFECTS OF LIDOCAINE AND K-Y JELLIES ON SORE THROAT, COUGH, AND HOARSENESS FOLLOWING ENDOTRACHEAL ANAESTHESIA
Doukumo DM*
Faponle AF†
Bolaji BO‡
Adenekan AT†
Olateju SOA†
*Departments of Anaesthesia, Obafemi Awolowo University Teaching Hospital, Ile-Ife, Nigeria,
†Departments of Anaesthesia, Obafemi Awolowo University, Ile-Ife, Nigeria,
‡Department of Anaesthesia, University of Ilorin, Ilorin, Nigeria.
E-mail: tonieadenekan@yahoo.com
Grant support: None
Conflict of Interest: None
ABSTRACT
Introduction: Tracheal intubation for general anaesthesia is often associated with postoperative sore throat, hoarseness and cough which can be distressing to patients. We compared the effects of lidocaine and K-Y jellies on postoperative sore throat, cough and hoarseness of voice following endotracheal anaesthesia.
Methods: Ninety-two ASA I or II patients scheduled for elective surgery under endotracheal general anaesthesia were randomly allocated into two groups. Tracheal tubes were lubricated with either 2% lidocaine jelly (LJ) or K-Y jelly (KYJ) for the groups and the patients were interviewed at 1, 12 and 24 hours post extubation.
Results: The mean scores for sore throat were lower in the KYJ group than the LJ group but this was only statistically significant at 12 hours (p = 0.02). The incidence of sore throat, hoarseness and cough were also lower in the KYJ than in the LJ group but these were not significant. While the incidence of sore throat was comparable among both sexes in the LJ group, it was higher in females (55.6%) than in males (18.8%) in the KYJ group (p = 0.02). Whereas in patients older than 30 years the incidence of sore throat, hoarseness and cough were similar in both groups, in patients less than 30 years, there were significant differences (p = 0.01 and 0.02 respectively). The incidence of side effects was similar in both groups irrespective of duration of intubation.
Conclusion: K-Y jelly is superior to lidocaine jelly in preventing postoperative sore throat, and in reducing the incidence of hoarseness of voice and cough. Postopearive throat complaints are more common in females than males.
Key words: Lidocaine jelly, K-Y jelly, Tracheal intubation, Postoperative complications, Sore throat, Hoarseness, Cough.
INTRODUCTION
Despite the developments in anaesthesia and surgery, major surgical operations are still associated with undesirable postoperative sequelae.1 These represent a significant negative aspect of surgical care, which may in no small way reduce the patient’s confidence in the healthcare system.1 Some of these postoperative sequelae are as a result of endotracheal intubation2 which is an integral part of anaesthetic practice to protect the airway from regurgitation and aspiration and provide a means of ventilation. Postoperative sore throat, cough and hoarseness of voice are common, uncomfortable, distressing sequelae after tracheal intubation.2 Throat irritation in the presence of an abdominal or thoracic incision can be very distressing especially in the presence of inadequate analgesia since any attempt to cough causes severe pain.
It has been postulated that these effects are due to mucosal injury with resulting inflammation caused by the process of airway instrumentation or the irritating effects of foreign objects like endotracheal tubes on the airway.3 Parts of the airway affected include the pharynx, larynx and trachea. Sore throat and hoarseness in the first 24 hours after surgery are among the most common complications of endotracheal intubation.4 Edomwonyi and colleagues5 reported that 63% of the general adult surgical population had postoperative throat complications. A higher incidence (72.5%) of postoperative airway complications was reported among obstetric and gynaecological population by Kolawole and Ishaq.1 A number of studies have shown that different factors correlate with the occurrence of these complications.6-9 These include: age, gender, season, anaesthetic drugs and gases, number of intubation attempts, duration of intubation, size and type of endotracheal tube, endotracheal tube cuff type and size, and site of surgery. Different measures including lubrication of endotracheal tubes with different types of gel are currently being tried to prevent or reduce the occurrence and severity of these throat complications following tracheal intubation.
Betamethasone, a water-soluble steroid that has been used topically for the treatment of inflammatory lesions of the oral mucosa has been consistently proven to reduce these airway complications.4,6,7 However, bethamethasone gel is not readily available in our environment. Lidocaine hydrochloride gel, 2% is indicated for prevention and control of pain in procedures. It is widely available and often used for lubrication of the endotracheal tubes before insertion, but it has not been found to be very helpful in the prevention of postoperative throat complications when used in the gel form.2,10 However, studies have revealed that intravenous lidocaine and lidocaine spray reduce these complications.7,11,12 K-Y jelly is a water-based, water-soluble lubricant which is biologically inert and contains no colour or perfume additives. K-Y jelly is widely used in medical practice as it does not stain and is easily cleaned up. Lidocaine and K-Y jellies are readily available in most health facilities in Nigeria, and are used interchangeably to lubricate endotracheal tubes before insertion.
To the best of our knowledge, there is currently no study from the West African sub-region that directly compares the influence of these two lubricants on the incidence and severity of postoperative sore throat, hoarseness and cough. This study was done to compare the effects of 2% lidocaine and K-Y jellies on the incidence and severity of sore throat, cough and hoarseness of voice following endotracheal anaesthesia. It was a prospective, randomized, double-blind study carried at a tertiary health facility over a period of four months in a semi-urban town in South-western Nigeria.
PATIENTS AND METHOD
Ninety-two consenting ASA physical status I or II adult patients scheduled for elective surgery under endotracheal general anaesthesia at the Obafemi Awolowo University Teaching Hospital at Ile-Ife, Nigeria over a period of four months were recruited for the study. Patients with upper respiratory tract infection or pre-existing history of throat pain, hoarseness and cough, those on steroid therapy and those who had nasogastric tube or throat packs inserted were excluded. Also excluded were patients in the following category: prolonged surgery (lasting more than 240 minutes), naso-tracheal intubation, anticipated difficult intubation, need for rapid sequence induction or re-intubation, head and neck surgery, operation in prone or lithotomy positions and patients with hyperactive airways such as asthmatics, smokers.
Following Institutional Ethics approval, the patients were randomly assigned to 2 groups of 46 patients each using paper balloting. The tracheal tubes of one group were lubricated with 2% lidocaine jelly (LJ) while the tubes for the second group were lubricated with K-Y jelly (KYJ). The low-pressure, high-volume single use cuffed polyvinyl chloride (PVC) tracheal tubes (Portex®) were lubricated from the distal end of the cuff to a distance of 15 cm from the tip using 2.5 ml of 2% lidocaine jelly or K-Y jelly spread uniformly while sterility was maintained. Size 8.0mm or 7.0mm internal diameter were used for male or female patients respectively. The name of the jelly used was not recorded on the anaesthesia chart, but was recorded separately with the patient’s code number.
Anaesthesia was induced with intravenous sodium thiopentone, and intubation facilitated with intravenous suxamethonium. Analgesia was provided with pentazocine 0.5mg/kg or tramadol 0.5-1mg/kg. All intubations were performed by experienced physician anaesthetists. The tracheal tube cuff was inflated with just enough room air to prevent an audible leak. Correct tube placement was confirmed by auscultation and the tube was secured with an adhesive tape. A single use oro-pharyngeal airway (size 3 or 4) was inserted and left in-situ throughout surgery. Anaesthesia was maintained with halothane 0.5–1% in oxygen/air mixture, and muscle relaxation was provided with intravenous pancuronium bromide 0.1mg/kg followed by top up doses as required. Ventilation was mechanically controlled using Drager Fabius Tiro (Drager Medical, AG and Company KG, 23542 Lubeck, Germany). Non-invasive monitoring including pulse oximetry, blood pressure, electrocardiography and temperature was performed on each patient using Dash 4000 multiparameter monitor (GE Medical System Information Technologies Inc., Wisconsin, USA). At the end of surgery, residual neuromuscular paralysis was reversed with a combination of neostigmine 0.05mg/kg and atropine 0.02mg/kg, the airway was gently suctioned under direct vision and extubation performed after return of the patient’s protective airway reflexes and satisfactory spontaneous tidal exchange. The patients were recovered in the post anaesthesia care unit and later transferred to the ward. A blinded anaesthetist interviewed all patients at 1, 12 and 24 hours post extubation.
Data collected included demographic details, perioperative vital signs, type of surgery, patient position during surgery, number of intubation attempts, duration of intubation, size and type of tube used and anaesthetic drugs used. Other data obtained were specific respiratory symptoms (sore throat, cough and hoarseness of voice) at 1, 12 and 24 hours post extubation and patient satisfaction after endotracheal intubation. Specific respiratory symptoms were scored on a four point Verbal Numerical Rating Scale (None = 0, Mild = 1, Moderate = 2, Severe = 3), and patient satisfaction was assessed with a four point verbal rating scale of Not satisfied, Slightly satisfied, Moderately satisfied and Very satisfied.
Data were presented as frequencies or proportions of total, means and standard deviations. Tests of significance were calculated using the chi-square for categorical data and student t-test for numerical data with the Statistical Package for the Social Sciences (SPSS) 16.0 for Windows Product. A p-value less than 0.05 was considered statistically significant.
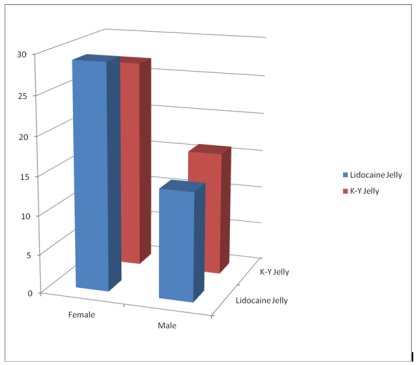
RESULTS Ninety-two patients who met the inclusion criteria were recruited for the study. Six of these (4 in LJ group and 2 in KYJ group) were excluded from analysis; four on account of prolonged surgery, and one each on account of intra-operative insertion of nasogastric tube and administration of lidocaine at induction for attenuation of pressor response to laryngoscopy and intubation. The demographic characteristics, number of intubation attempts, and duration of intubation for the two groups were similar as shown in Table I. Baseline and intraoperative vital parameters of the two groups were similar. Figure 1 shows the sex distribution and Figure 2 shows the type of surgery performed on the patients. The mean sore throat score was generally lower in the K-Y jelly group compared to the lidocaine jelly group and the difference was statistically significant at 12 hours post-extubation (p = 0.02) as shown in Table 2. The mean scores for hoarseness and cough for the two groups were similar.
The incidence of sore throat, hoarseness and cough is shown in Table 3. For sore throat, the incidence was generally lower in the KYJ group though not significantly (p = 0.47, 0.05 and 0.24 at 1, 2 and 12 hours respectively). It ranged from 20.9 - 34.9% in the LJ group and from 11.6 - 23.3% in the KYJ group within the 24-hour study period. The highest incidence of sore throat occurred at 1 hour in the KYJ group (23.3%) and at 12 hours in the LJ group (34.9%).
Though the incidence of hoarseness was lower in the KYJ group than in the LJ group, there were no significant differences (p = 0.80, 0.48 and 1.00 at 1, 12 and 24 hours respectively). The highest incidence of hoarseness occurred at 1 hour in both groups and the incidence thereafter reduced with time. The incidence of cough was lower in KYJ group than in the LJ group at 1 and 12 hours. It was however higher at 24 hours and these were not statistically significant. The highest incidence of cough occurred at 1 hour in the LJ group (27.9%) and at 12 hours in the KYJ group (23.3%).
The effects of age, gender and duration of intubation on the incidence of postoperative sore throat, hoarseness and cough among the two groups are shown in Tables 4, 5 and 6. The incidence of sore throat was comparable among both sexes in the lidocaine jelly group (p = 0.72) but was significantly higher in females (55.6%) than in males (18.8%) in the K-Y jelly group (p = 0.02). In patients older than 30 years, the incidence of sore throat, hoarseness and cough were similar in both groups (p = 0.44, 0.61 and 0.12 respectively). While in patients aged 30 years old or less, the incidence of sore throat was similar in both groups (p = 0.26), the incidence for hoarseness and cough were significantly higher in the LJ group than in the KYJ group (p = 0.01 and 0.02 respectively). The incidences of sore throat, hoarseness and cough were similar in both groups irrespective of the duration of endotracheal intubation. Patients’ satisfaction in both groups was similar (p = 0.55).
DISCUSSION
The finding of this study suggests that 2% lidocaine jelly offers no advantage over K-Y jelly in preventing postoperative airway complications. K-Y jelly was associated with a significantly lower mean sore throat scores at 12 hours postoperatively compared with lidocaine jelly. The incidence of sore throat at 1, 12, and 24 hours after surgery were lower in the K-Y jelly group compared with the lidocaine group. Although the differences were not statistically significant, a study involving a larger number of patients may be able to show some significant differences between the two.
Selvaraj and Dhanpal13 compared steroid gel with lidocaine jelly and a control group with nothing applied to the tube and found the incidence of sore throat to be 33.3% in the steroid gel group versus 73.3% in the other two groups. They reported that the incidence of cough and hoarseness was 23.3% in the steroid gel group, 63.3% in the lidocaine gel group and 50% in the control group. Their study also suggested that lidocaine jelly increased the incidence of these symptoms when compared with the control group and demonstrated that steroid gel reduced the incidence of the symptoms significantly when compared with lidocaine gel. A similar finding was reported by Kori and colleagues10 who studied the influence of endotracheal tube cuff lubrication with lidocaine jelly on postoperative sore throat and hoarseness. Their finding suggested that lidocaine jelly reinforced the severity of sore throat compared to their no intervention group in agreement with the report of Selvaraj and Dhanpal13, and that lidocaine sprayed to the trachea did not reduce postoperative sore throat. The effect of lidocaine on postoperative airway complications is summarised by McHardy and Chung14 in their review on postoperative sore throat where they noted that no study has categorically demonstrated that the use of lubricating jelly containing a local anaesthetic is beneficial in the reduction of postoperative sore throat after tracheal intubation.
Kazemi and Amini4 studied the effects of betamethasone gel in reducing airway complications after endotracheal anaesthesia, using K-Y jelly as control. They reported a significant reduction in incidence and severity of sore throat, hoarseness and cough postoperatively in the betamethasone group compared with the K-Y gel group. The same beneficial effect has been reported by other researchers concerning betamethasone and other steroids including their inhalational preparations.13,15,16 Steroid gel has been found to be far superior to local anaesthetic jelly because of the anti-inflammatory property but steroids do not abort all the throat complications. This suggests that the causative factors of postoperative throat complications are multi-factorial. These other factors should therefore be elucidated in order to find measures aimed at reducing them.
We found the overall incidence of sore throat, hoarseness and cough following endotracheal anaesthesia after lubricating the tracheal tube with lidocaine jelly to be 34.9%, 25.6%, 27.9% respectively and with K-Y jelly, 16.3%, 23.3% and 18.6% respectively. After tracheal intubation, the incidence of sore throat varies from 14.4% to 50%.14 Our reported incidence is lower than that reported by Maruyama and colleagues7 who studied 418 adult surgical patients, and assessed possible factors associated with sore throat and hoarseness after total intravenous anaesthesia. They reported overall incidence of 50% and 55% for sore throat and hoarseness respectively. Head and neck surgeries known to be associated with tube movement during surgery and consequently increased risk of postoperative airway complications were included in their study. Our incidence is comparable with those reported by Edomwonyi and colleagues5 for sore throat (31%), cough (22%) and hoarseness (9.5%) in their study of 200 consecutive adult patients who presented for surgery. However, certain cases associated with known risk factors for postoperative airway complications including use of nasogastric tubes, throat packs, head and neck surgeries were included in their series. Their exclusion criteria were patients with preoperative sore throat or throat complications.
Our study showed that significantly more females had sore throat compared to the males in both study groups though smaller sized 7.0mm ID tubes were used in females while larger sized 8.0mm ID tubes were used in males. This observation supports previous studies showing that the female gender is at a greater risk for postoperative airway complications.17,18 This has been attributed to the tube often being of a tighter fit in females.14,19 This study had some limitations. The sample size used in this study was small and this limited the statistical significance of some of the findings. The endotracheal tube cuff pressure could not be measured in this study because of the lack of appropriate equipment. A constant cuff pressure was therefore not maintained and could be a source of error.
Postoperative analgesia used was also not standardised and may have influenced the perception and reporting of postoperative airway complaints.
In conclusion, this study has demonstrated that K-Y jelly is superior to lidocaine jelly in preventing postoperative sore throat and reducing the incidence of hoarseness of voice and cough particularly in young adults. Lidocaine jelly is associated with increased incidence of postoperative throat complaints. This study also confirmed that postoperative throat complaints are more common in females than males.
REFERENCES
- Kolawole IK, Ishaq MS. Post-anaesthetic respiratory complaints following Endotracheal Anaesthesia in lower abdominal obstetrics and gynaecology surgery. Nig J Clinic Pract 2008; 11: 225 – 230.
- Sumathi PA, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between Betamethasone gel and Lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough and hoarseness of voice. Br J Anaesth 2008; 100: 215 - 218.
- Scuderi PE. Postoperative Sore Throat: More Answers Than Questions. Anesth Analg 2010; 111: 831 - 832.
- Kezemi A, Amini A. The effect of bethamethasone gel in reducing sore throat, cough and hoarseness after laryngotracheal intubation. Middle East J Anesthesiol 2007; 19: 197-204.
- Edomwonyi NP, Ekere IT, Omo E, Rupasinghe A. Postoperative throat complications after tracheal intubation. Ann Afr Med 2006; 5: 28 – 32.
- El Hakim M. Beclomethasone prevents postoperative sore throat. Acta Anaesth Scand 1993; 37: 250 – 252.
- Honarmand A, Safavi M. Bethamethazone inhaler versus intravenous lidocaine in the prevention of postoperative airway and throat complaints: a randomized, controlled trial. Ann Saudi Med 2008; 28: 11 - 16.
- Canbay O, Celebi N, Sahin A, Celiker V, Ozgen, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth 2008; 100: 490 – 493.
- Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur J of Anaesthesiol 2005; 22: 307 – 311.
- Kori K, Muratani T, Tatsumi S, Minami T. Influence of endotracheal tube cuff lubrication on postoperative sore throat and hoarseness. Masui 2009; 58: 342 - 345.
- Takekawa K, Yoshimi S, Kinoshita Y. Effects of intravenous lidocaine prior to intubation on postoperative airway symptoms. J Anesth 2006; 20: 44 - 47.
- Honma K, Kamachi M, Akamatsu Y, Yoshioka M, Yamashita N. Lidocaine spray 10 min prior to intubation: effects on postoperative sore throat. J Anesth 2010; 24: 962 - 965.
- Selvaraj T, Dhanpal R. Evaluation of the application of topical steroids on the endotracheal tube in decreasing post-operative sore throat. J Anaesth Clin Pharmacol2002; 18: 167 - 170.
- McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999; 54: 444 – 453.
- Tazeh-kand NF, Eslami B, Mohammadian K. Inhaled Fluticasone Propionate Reduces Postoperative Sore Throat, Cough, and Hoarseness. Anesth Analg 2010; 111: 895 – 898.
- Ayoub MC, Ghobashy A, McGrimley L, Koch ME, Qadir S, Silverman DG. Wide spread application of topical steroids to decrease sore throat, hoarseness and cough after tracheal intubation. Anesth Analg 1998; 87: 714 - 716.
- Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth 2002; 88: 582 – 584.
- Ahmed A, Abbasi S, Ghafoor HB, Ishaq M. Postoperative sore throat after elective surgical procedures. J Ayub Med Coll Abbottabad 2007; 19: 12 - 14.
- Zuccherelli L. Postoperative upper airway problems. SAJAA 2003; 9: 12 - 16.
| Table 1: Demographic characteristics, number of intubation attempts, and duration of intubation for the two groups |
|
Characteristics |
Lidocaine |
K-Y |
p – value |
|
Age (years) |
42.40 ± 15.74 |
41.07 ± 12.29 |
0.66‡ |
|
Weight (kg) |
66.84 ± 13.87 |
70.05 ± 13.48 |
0.28‡ |
|
No. of intubation attempts |
1.30 ± 0.71 |
1.09 ± 0.29 |
0.08‡ |
|
Duration of intubation (mins) |
138.74 ± 44.33 |
136.67 ± 55.67 |
0.85‡ |
| Table 2: Mean scores for sore throat, hoarseness and cough |
|
Time after extubation. (hrs) |
Lidocaine |
K-Y |
p – value |
|
Sore throat score 1 hr |
0.42 ± 0.73 |
0.28 ± 0.55 |
0.32‡ |
|
12 hrs |
0.49 ± 0.80 |
0.16 ± 0.37 |
0.02† |
|
24 hrs |
0.28 ± 0.60 |
0.12 ± 0.32 |
0.12‡ |
|
Hoarseness score |
|
|
|
|
1 hr |
0.30 ± 0.56 |
0.33 ± 0.64 |
0.86‡ |
|
12 hrs |
0.24 ± 0.62 |
0.12 ± 0.32 |
0.26‡ |
|
24 hrs |
0.05 ± 0.21 |
0.05 ± 0.21 |
1.00‡ |
|
Cough score |
|
|
|
|
1 hr |
0.33 ± 0.57 |
0.21 ± 0.47 |
0.30‡ |
|
12 hrs |
0.33 ± 0.61 |
0.28 ± 0.55 |
0.71‡ |
|
24 hrs |
0.14 ± 0.47 |
0.21 ± 0.41 |
0.46‡ |
| Table 3: Incidence of sore throat, hoarseness and cough at 1, 12, and 24 hours post-operation |
|
|
Sore throat |
|
|||
|
|
Lidocaine Jelly |
K-Y Jelly |
|
||
|
Time after extubation. (hrs) |
Yes |
No |
Yes |
No |
p-value |
|
1 |
13 (30.2%) |
30 (69.8%) |
10 (23.3%) |
33 (76.7%) |
0.47‡ |
|
12 |
15 (34.9%) |
28 (65.1%) |
7 (16.3%) |
36 (83.7%) |
0.05‡ |
|
24 |
9 (20.9%) |
34 (79.1%) |
5 (11.6%) |
38 (88.4%) |
0.24‡ |
|
|
Hoarseness |
|
|||
|
|
Lidocaine Jelly |
K-Y Jelly |
|
||
|
Hours |
Yes |
No |
Yes |
No |
p-value |
|
1 |
11(25.6%) |
32(74.4%) |
10(23.3%) |
33(76.7%) |
0.80‡ |
|
12 |
7(16.7%) |
35(83.3%) |
5(11.6%) |
38(88.4%) |
0.48‡ |
|
24 |
2(4.7%) |
41(95.3%) |
2(4.7%) |
41(95.3%) |
1.00‡ |
|
|
Cough |
|
|||
|
|
Lidocaine Jelly |
K-Y Jelly |
|
||
|
Hours |
Yes |
No |
Yes |
No |
p-value |
|
1 |
12(27.9%) |
31(72.1%) |
8(18.6%) |
35(81.4%) |
0.31‡ |
|
12 |
11(25.6%) |
32(74.4%) |
10(23.3%) |
33(76.7%) |
0.80‡ |
|
24 |
4(9.3%) |
39(90.7%) |
9(20.9%) |
34(79.1%) |
0.13‡ |
| Table 4: Effect of age, gender and duration of intubation on postoperative sore throat |
|
|
|
Number |
No Yes |
p – value |
|
|
Age (years) |
> 30 L |
33 |
17 (51.5%) |
16 (48.5%) |
0.44‡
0.26‡
|
|
|
K-Y ≤ 30 L K-Y |
26
10 17 |
16 (61.5%)
8 (80.0%) 10 (58.8%) |
10 (38.5%)
2 (20.0%) 7 (41.2%)
|
|
|
Gender |
L Male Female K-Y Male |
14 29
16 |
9 (64.3%) 17 (58.6%)
13 (81.2%) |
5 (35.7%) 12 (41.4%)
3 (18.8%) |
0.72‡
0.02† |
|
|
Female |
27 |
12 (44.4%) |
15 (55.6%)
|
|
|
Duration of intubation (minutes) |
> 60 min L K-Y |
39 40 |
24 (61.5%) 22 (55.0%) |
15 (38.5%) 18 (45.0%) |
0.56‡
0.15‡
|
|
|
≤ 60 min L K-Y |
4 3 |
2 (50.0%) 3 (100%)
|
2 (50.0%) 0 (0%) |
|
|
†- Statistically significant ‡ - Not statistically significant |
|||||
| Table 5: Effect of age, gender and duration of intubation on postoperative hoarseness |
|
|
|
Number |
No |
Yes |
p – value |
|
Age (years) |
> 30 L K-Y |
33 26 |
24 (72.7%) 19 (73.1%) |
9 (27.3%) 7 (26.9%) |
0.61‡
0.01† |
|
|
≤ 30 L K-Y |
10 17 |
3 (30.0%) 14 (82.4%)
|
7 (70.0%) 3 (17.6%) |
|
|
Gender |
L Male Female K-Y Male |
14 29
16 |
8 (57.1%) 15 (51.7%)
12 (75.0%) |
6 (42.9%) 14 (48.3%)
4 (25.0%) |
0.74‡
0.11‡ |
|
|
Female
|
27 |
25 (92.6%) |
2 (7.4%) |
|
|
Duration of intubation (minutes) |
> 60 min L K-Y |
39 40 |
25 (64.1%) 29 (72.5%) |
14 (35.9%) 11 (27.5%) |
0.42‡
|
|
|
≤ 60 min L K-Y |
4 3 |
3 (75.0%) 3 (100%) |
1 (25.0%) 0 (0%) |
0.35‡ |
| Table 6: Effect of age, gender and duration of intubation on postoperative cough |
|
|
|
Number |
No |
Yes |
p – value |
|
Age (years) |
> 30 L K-Y |
33 26 |
23(69.7%) 13(50.0%) |
10(30.3%) 13(50.0%) |
0.12‡
0.02† |
|
|
≤ 30 L K-Y |
10 17 |
4(40.0%) 14(82.4%) |
6(60.0%) 3(17.6%)
|
|
|
Gender |
L Male Female K-Y Male |
14 29
16 |
7(50.0%) 18(62.1%)
13(81.2%) |
7(50.0%) 11(37.9%)
3(18.8%) |
0.45‡
0.14‡ |
|
|
Female |
27 |
16(59.3%) |
11(40.7%)
|
|
|
Duration of intubation |
> 60 min L K-Y ≤ 60 min L K-Y |
39 40
4 3
|
26(66.7%) 24(60.0%)
2(50.0%) 2(66.7%) |
13(33.3%) 16(40.0%)
2(50.0%) 1(33.3%) |
0.54‡
0.66‡
|
Figure 1: Showing the Sex distribution of the patients
p = 0.65
Figure 2: Showing the type of Surgeries performed on the patients